Most burn injuries can be managed on an outpatient basis by primary care physicians. Prevention efforts can significantly lower the incidence of burns, especially in children. Burns should be managed in the same manner as any other trauma, including a primary and secondary survey.
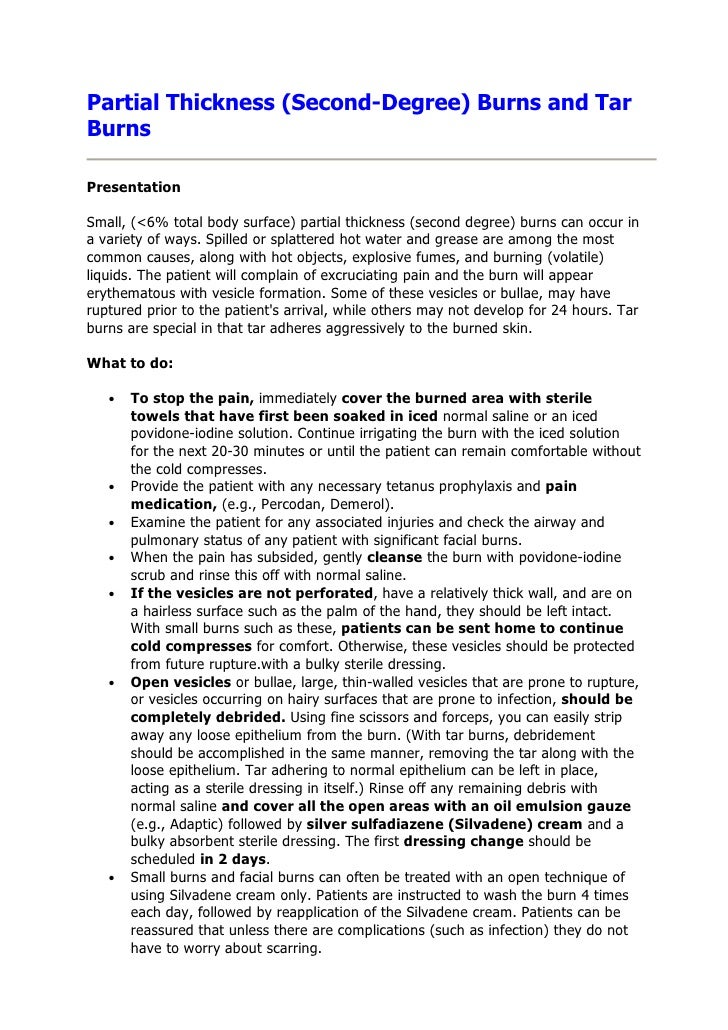
Superficial burns can be treated with topical application of lotions, honey, aloe vera, or antibiotic ointment. Partial-thickness burns should be treated with a topical antimicrobial agent or an absorptive occlusive dressing to help reduce pain, promote healing, and prevent wound desiccation. Topical silver sulfadiazine is the standard treatment; however, newer occlusive dressings can provide faster healing and are often more cost-effective.
Physicians must reevaluate patients frequently after a burn injury and be aware of the indications for referral to a burn specialist. Topical antimicrobial agents for the burn wound were developed in the 1950s and 1960s to deal with the problem of invasive infection of the burn wound. Invasive infection of the burn wound leading to sepsis and death was commonplace . Aside from the recognized threat of burn wound sepsis, burn wound infections also may lead to wound conversion, skin graft failure, and prolonged hospitalization. The introduction of topical antimicrobial agents was a major advancement in burn care and proved to be responsible for important reductions in mortality from burn wound sepsis .
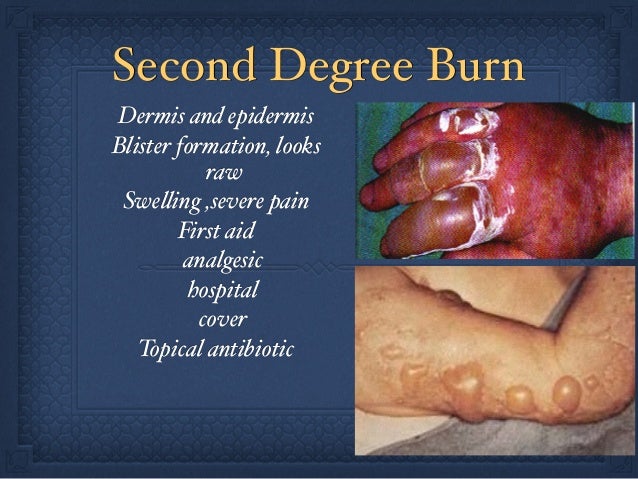
Therefore, regardless of burn depth, topical antimicrobials are most importantly indicated when there is clinical suspicion of risk of infection, or when a wound infection is evident. Second degree burns can be more serious and thus require more care than first degree burns. First, cool the wound under running water for 10 to 15 minutes.
Do not apply ice or extremely cold water as it could create further damage and lower the body's temperature. Use the Hansaplast Wound Sprayto clean from bacteria to prevent infections. Do not attempt to break any blisters that may occur.
Many second-degree burns will heal within a week or two if kept clean and cared for. Application of a topical antimicrobial agent to a burn wound is now a standard intervention that contributes to improved outcome following burn injury. However, the wide variety of available agents makes the choice of an appropriate agent quite challenging, especially in children with burns. The deep second-degree burn in a child poses a more difficult challenge. The difficulty mainly arises from our imprecision in diagnosing this burn depth.
However, If the burn is truly a deep partial-thickness wound, there is a higher risk of a burn wound infection and early excision and grafting is the recommended approach. One practical consideration in this scenario is that SSD and mafenide cream leave a pseudoeschar on the wound which makes ongoing assessment of the burn depth even more difficult. This problem could be avoided with the 5% mafenide acetate solution.
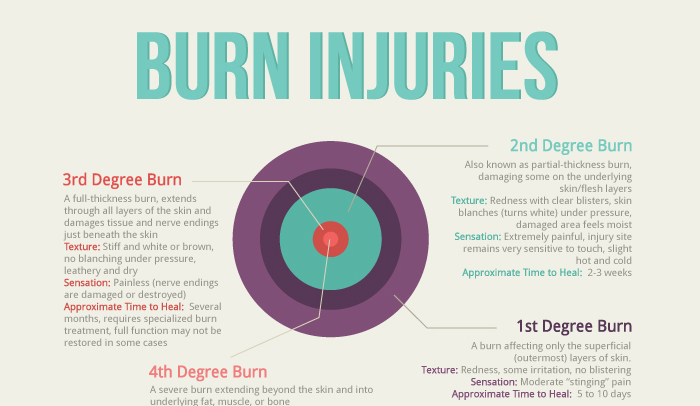
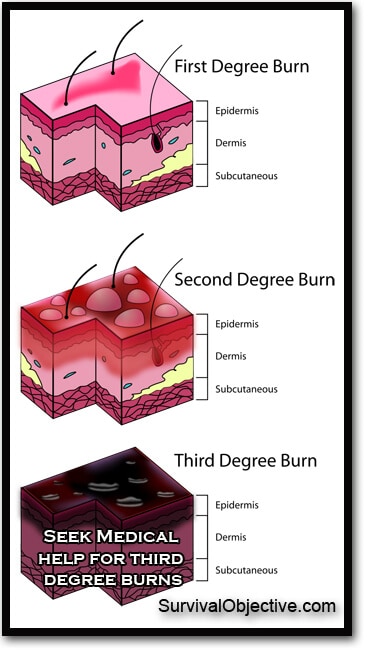
Antiseptic solutions such as Dakin's or acetic acid may also be considered but are less conventional. Nanocrystalline silver-releasing dressings such as Acticoat® may also be a useful option as they require less frequent changes and do not produce a pseudoeschar. When diagnosing a burn, a doctor evaluates the depth and extent of the damage, the degree of pain, the amount of swelling, and signs of infection. Doctors classify the burn based on the depth and extent of the injury.
In the emergency room, all wounds are wrapped with sterile cloths. People with burns are also evaluated for associated injuries . Doctors may also conduct tests to determine whether the wound is infected.
Third-degree and more severe burns damage both layers of the skin and may also damage the underlying bones, muscles, and tendons. Sometimes there is no pain because the nerve endings under the skin are destroyed. Third-degree burns have a high risk of infection. This surgery, done with general anesthesia, removes the injured skin and replaces it with healthy skin from an uninjured area of the body. Full thickness burns that are not grafted may take months or even years to heal.
Burn survivors may have a combination of first, second, and third degree burns. Talk with your health care providers to better understand your specific injuries. Although early debridement and closure are strongly recommended for deep dermal and full-thickness burns, there are situations where early surgical excision cannot be performed. Under these circumstances, the application of cerium nitrate , a salt compound of the rare earth element cerium, to these wounds may be beneficial.
The first is that application turns burn eschar into a dry, hard, and adherent "shell" that protects the underlying wound from bacterial invasion. Eventually, when surgical excision of this cerium-hardened eschar is performed, the underlying granulation tissue is typically clean and suitable for grafting upon. However, older literature has found conflicting results with respect to CN's effects on mortality . Many topical antimicrobial agents are cytotoxic to keratinocytes and fibroblasts, and as such have the potential to delay wound healing . In practical terms, among more superficial burns that are expected to heal on their own, it is more important to strike this balance.
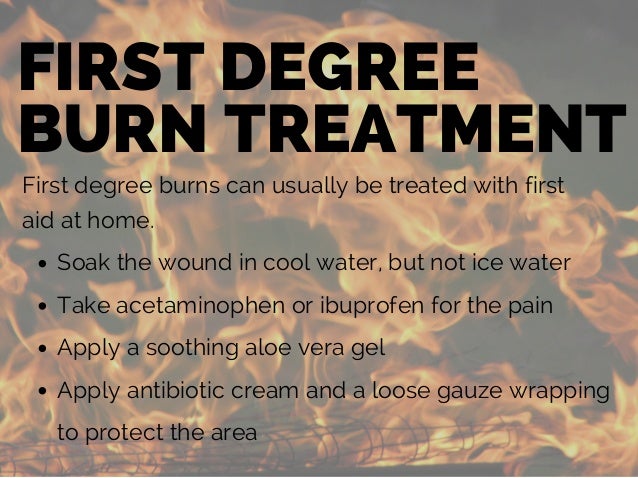
In these burns the goal is healing within 2–3 weeks of injury to reduce the likelihood of hypertrophic scarring . In the event that you suffer a first-degree burn, soak the burn in cool water for about 5 minutes – this helps reduce swelling by pulling the heat away from burned skin. Then, treat the skin with Aloe Vera or antibiotic ointment and wrap it loosely in a dry gauze bandage. An over-the-counter pain reliever can also help with the pain and swelling. This capability was originally harnessed to successfully counter the problem of invasive burn wound infection and fatal septicemia from gram-negative species, especially Pseudomonas . The agent was initially produced as an 11% cream, but is also available as a 5% aqueous solution.
The most common use of mafenide acetate is for deep or infected burns where penetration of the antibiotic into the eschar is advantageous. For the same reason, the cream is also used for deep burns of the ear to prevent invasive infection leading to suppurative chondritis of the ear cartilage . In contrast, deeper burns are covered by an avascular layer of moist and protein-rich dead skin , which fosters bacterial proliferation and invasion, leading to burn wound infection. Furthermore, generalized immunosuppression associated with major burn injuries predisposes the patient to local burn wound infection. When bacteria in the eschar penetrate surrounding uninjured tissues and invade the bloodstream, fatal sepsis may result. Many people mistakenly apply ice to burns because it feels soothing, but ice can cause more harm than good in burn cases.
Ice should not be applied to burns as it may cause nerve damage and frostbite, especially with more severe burns where the nerve may already be exposed. Using ice after the initial burn may slow the healing the process further and cause more damage to the surrounding skin. Instead of ice, run cold water over the burn for several minutes following the initial burn. If you are unsure of first aid after a burn, it is always best to seek medical attention.
Antibiotic (an-ti-bahy-OT-ik) ointments or creams are often used to prevent or treat infections in patients with second-degree burns. Using these ointments may require the use of bandages. Your doctor can assist you in coordinating the dressing changes with your pain medication. Dressings can be soaked off with water in a sink or shower.
The skin and the burn wound should be washed gently with mild soap and rinsed well with tap water. Use a soft wash cloth or piece of gauze to gently remove old medications. A small amount of bleeding is common with dressing changes.
Your doctor will decide on the appropriate dressing and ointment. This will be based on the location of the burn, the need to control drainage, and your comfort. Superficial burns, like sunburns, are commonly red and painful. If it's a superficial burn, immediate medical care might not be necessary. If you or your child suffers a minor burn, it will appear red, a little swollen, and it will turn white when you press on the skin.
A minor burn is painful – soothe the pain by cooling the burn under cool, not cold, running water for 10 to 15 minutes. You can also apply a clean towel dampened with cool water to the burn. Ice is not recommended as an initial treatment for burns because it can decrease circulation and make the burn worse. Do not put any food-based products on the burn as this may cause infection and make it more difficult to clean the wound.
Treat small burns with over-the-counter topical antibiotic ointment, like Polysporin or Neosporin, until healed. Burns heal better in a moist, covered environment. First degree and smaller second degree burns are usually managed well at home. First aid may include soaking the burned area in clean cool water for a few minutes to stop the burning process, and then drying gently. Creams, such as aloe vera or burn ointments may help relieve some of the pain or discomfort. Keep the burns clean and loosely covered, and monitor for breaks in the skin and signs of infection.
Whether you burn your hand on a pan of cookies, spend too much time in the sun, or spill hot coffee on your lap, burns are certainly not pleasant. Unfortunately, burns are one of the most common household injuries. A first-degree burn is considered the least severe because it only affects the outer layer of skin. It usually only causes mild pain, redness, and swelling.
Second-degree burns affect deeper layers of the skin and cause blisters and white, wet, and shiny skin. Third-degree burns involve damage to all layers of the skin, while fourth-degree burns may involve the joints and bones. Third- and fourth-degree burns are considered medical emergencies and should only be treated in a hospital. You can treat most first-degree burns and second-degree burns less than 3 inches in diameter at home. Read on to learn which remedies are best for healing your skin, and also which remedies should be avoided. An antibiotic ointment contains an antibiotic within a water-in-oil emulsion where the volume of oil exceeds that of the water.
Thus, such ointments provide not only an antibacterial effect but also they create a moist wound healing environment. Hence, these agents are optimally suited for superficial burns where spontaneous healing is expected. While the spectrum of bacterial coverage tends to be limited, these agents are relatively free of complications.
In general, the ointments are applied two to three times daily as a thick layer for moisture retention and then are covered with a non-adherent dressing layer followed by gauze . Mostly they are soothing to apply, easier to clean off than creams such as SSD, and tend to be reasonably well tolerated by children. One problem with MA is its lack of antifungal activity. Addition of nystatin to MA is used to avoid fungal overgrowth with prolonged use of MA. Another disadvantage is that MA is painful on application, especially on more superficial wounds.
To some extent, this problem has been reduced by using the 5 and 2.5% solutions . Like other topical antimicrobials, MA is cytotoxic to fibroblasts and keratinocytes and may impede wound healing. In vitro studies suggest that concentrations as low as 0.1% are toxic to these cells . For this reason, mafenide acetate cream is usually reserved for smaller deep burns, or it is alternated with SSD on larger burns. Acid-base disturbances were not seen with use of the 5% solution in a study of nearly 700 adult and pediatric burn patients . Finally, MA may occasionally cause a local rash or skin irritation .
Paradoxically, many of the topical antimicrobial agents currently in use also have cytotoxic effects on keratinocytes and fibroblasts and have the potential to delay wound healing. Especially relevant to the pediatric burn patient are the antimicrobial agent's properties related to causing pain or irritation and the required frequency of application and dressings. This article will discuss the general principles surrounding the use of topical antimicrobials on burn wounds and will review the most common agents currently in use.
Most first-degree burns are relatively minor and are most often caused by brief contact with a hot surface or a minor scald from hot water. Another common form of first-degree burn is sunburn, caused by damage from the sun's UV rays. Typically, first degree burns recover on their own and do not require special treatment. However, it is recommended to cool the affected area under running water to relieve the pain and then apply Hansaplast Wound Healing Ointment. If you have a sunburn, wear loose-fitting clothing for a few days and drink plenty of fluids to stay hydrated. Mepilex AG gray foam covered with a minimal amount of gauze and netting.
NOT ADVISED FOR HOME DRESSING CHANGES. Changed at least weekly at the burn center or primary care clinic. This type of dressing takes advantage of the antibiotic properties of silver and can be cut to fit the patient's needs and can be used on partial thickness burns. Consider this for children who would benefit from less frequent changes. A first degree burn, while still painful, can normally be treated as a minor burn. First degree burns directly damage only the epidermis, the outermost layer of the skin, and whilst there may be pain, redness or swelling, it's not very serious and can be treated at home.
It generally has a low risk of infection and scarring. Most sunburns are also first degree burns and can be treated much the same way as other minor burns. A second-degree burn is more serious, causing red, white or splotchy skin, swelling, pain and blisters.
If you suffer a small second-degree burn that is no larger than 3 inches, you can follow the same course of self-treatment, but just holding the burn in cool water for about 15 minutes. However, if the burned area is larger or covers the hands, feet, face, groin, buttocks or a major joint, treat it as a major burn and seek immediate medical treatment. Third degree burns result in damage to all of the layers of the skin and require immediate medical attention.





















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.